
Treatments available for vulvovaginal candidiasis, more commonly referred to as vaginal yeast infection, include antifungal drugs in intravenous and pill formulations. But fungi are developing resistance to these older medicines, making them less effective. The FDA this week approved an antifungal from Scynexis, providing a new treatment option that also represents the first new antifungal drug class in 20 years.
The Scynexis antifungal, ibrexafungerp, is available as a pill. It will provide an alternative to fluconazole, a decades-old antifungal that is the only other oral antifungal available for treating vaginal yeast infections. Jersey City, New Jersey-based Scynexis will market its drug—the company’s first FDA-approved product—under the trade name “Brexafemme.”
Antifungal drugs work by interfering with some key part of a fungal cell. Brexafemme blocks glucan synthase, an enzyme that is an essential component of the fungal cell wall. The 2001 FDA approval of echinocandins made that class of antifungals the newest one until this week. Those drugs also block glucan synthase. But echinocandins are intravenously administered so they must be given in a clinical setting. As a pill, Brexafemme can be taken in a hospital or at home. The recommended dose is four pills taken in one day—two 150 mg pills in the morning and then two more 150 mg pills taken about 12 hours later.
Fluconazole, the other FDA-approved oral medication for treating yeast infections, targets a different enzyme. According to Brexafemme’s prescribing information, the drug retains its antifungal activity at the 4.5 pH that is the normal vaginal pH level. The paperwork also notes that Brexafemme retains its activity against most species of Candida fungi that have developed resistance to fluconazole.
The FDA based its Brexafemme approval decision on the results of two placebo-controlled Phase 3 studies enrolling more than 500 patients combined. The main goal was to measure the percentage of patients that achieved a clinical cure—a complete resolution of the signs and symptoms of infection. According to a Scynexis investor presentation, 50.5% of patients achieved that goal in the first Phase 3 study compared to 28.6% of those given a placebo. In the second Phase 3 clinical trial, 63.3% of patients achieved the main study goal compared to 44% of those who received a placebo. Those results were statistically significant.
In all of the clinical trials testing Brexafemme, Scynexis reported no systemic problems associated with its drug. Most of the treatment-related adverse events reported were gastrointestinal (diarrhea, nausea, abdominal pain); 85% of them were classified as mild and half of them lasted a day or less.
Scynexis discovered ibrexafungerp under a research collaboration with Merck. Following a review of its infectious diseases portfolio, the pharma giant transferred all of its rights to the program to Scynexis in 2013. Under the agreement, Scynexis must pay Merck royalties from sales of its drug.
The FDA approval of Brexafemme enabled Scynexis to beat several other biotechs to the market with an oral alternative to the older antifungals used to treat vulvovaginal candidiasis. Durham, North Carolina-based Mycovia Pharmaceuticals has advanced its pill, oteseconazole, through pivotal testing and expects to file for FDA approval in the first half of this year. Amplyx, a San Diego-based antifungal biotech with a novel antifungal candidate in mid-stage clinical development, was acquired by Pfizer earlier this year. No financial terms of the acquisition were disclosed.
Scynexis will commercialize Brexafemme through a partnership with Amplity Health, a contract commercialization organization. The drug is expected to launch in the second half of this year.
Additional Scynexis studies that could expand Brexafemme’s label are underway. The company is conducting a Phase 3 clinical trial that is testing the drug as a preventative measure for recurrent vulvovaginal candidiasis; the company expects a supplemental new drug application could be filed for that indication in the first half of next year.
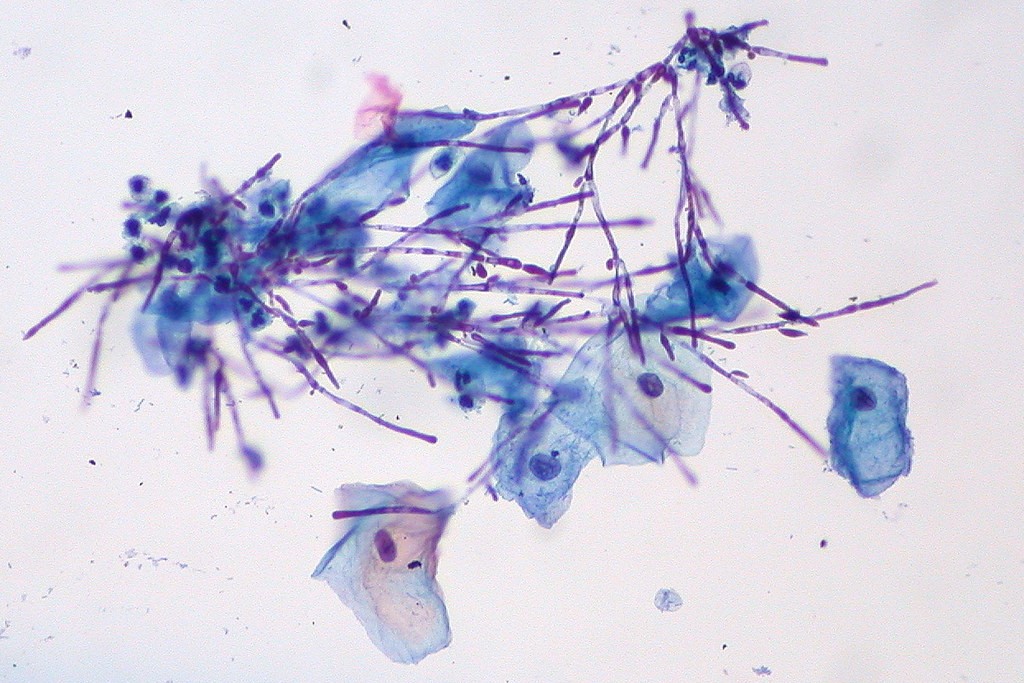
Photo by Flickr user Ed Uthman via a Creative Commons license


















