Nurses have always faced unique and complex challenges. In 2022, these challenges were exacerbated by acute and ongoing staffing shortages, demographic changes, bureaucratic and managerial demands, tight budgets, stress, burnout, and cultural shifts (including an increase in travel nurses and temporary assignments). These factors can put nurses and their patients at considerable risk.
Nurses have always faced unique and complex challenges. In 2022, these challenges were exacerbated by acute and ongoing staffing shortages, demographic changes, bureaucratic and managerial demands, tight budgets, stress, burnout, and cultural shifts (including an increase in travel nurses and temporary assignments). These factors can put nurses and their patients at considerable risk.
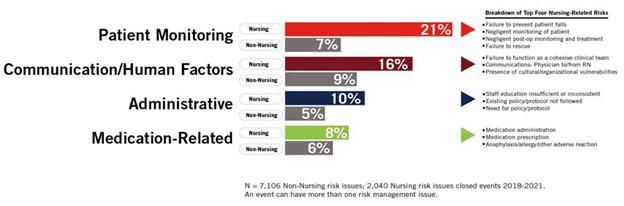
To assess nursing vulnerabilities, Coverys evaluated 4,634 medical malpractice claims that closed between 2018 and 2021 and identified 850 specific events where nurses were directly involved in the alleged medical error. We determined the root causes of these incidents and used our analysis to point to notable risk trends. The conclusions are not absolute findings. Rather, they are hypotheses based on the data—forewarnings from the past about where vulnerabilities existed and may still be at play.
Top Risk Issues in Nursing
The top risks for nursing-related events occurred at a much higher rate than claims that did not involve nurses.
Themes & Trends
The data yielded clear themes and trends when it comes to nursing-related risks:
- Comprehensive information is critical to successful caregiving. Mistakes are more likely to happen in the absence of details about a patient’s medical history, such as the presence of comorbidities, allergies, and other important factors. Nurses need to know: “What is this patient’s story?” The story can be curated in many ways: consulting the electronic health record and updating it along the way; speaking directly to the patient and their other providers; keenly observing a patient’s behaviors and symptoms; and asking critical questions.
- Insufficient staffing is the root of most preventable adverse events. While clinical judgment is imperative, the common denominator in a vast number of adverse nursing events is a lack of proper staffing. Mistakes happen when there are too many patients to care for; when the nurse must leave one patient unattended to rush to another bedside; when the caregiver is distracted while administering medication; and when there’s no access to assistance—up, down, or across the chain of command. Caring for too many patients and doing so under intense pressure can lead to missed critical processes (such as checking the EMR for allergies or lab results).
- Ongoing assessment and training are imperative. Nursing-related claims often involve an avoidable gap in knowledge, such as lack of proper training on how to assess skin integrity or administer uncommon medications. Hospitals and medical practices that focus on best practices and provide training on important nursing skills inevitably create safer environments. It’s also imperative to regularly assess the skills of both staff and travel nurses.
- Nurse empowerment is key to patient-safety. Many nurses are not sufficiently encouraged to speak up when they have a concern. Cultural deficiencies can make entire teams fear retribution or blame for questioning authority or reporting an error. Institutions that empower their nurses and amplify their voices can significantly improve patient safety.
- Some patient populations are at higher risk than others. Our data shows that some patients are at a higher risk for adverse nursing events. These include elderly or unaccompanied patients; patients with language, health literacy, or cultural barriers; patients requiring close monitoring (like post-operative patients); patients with polypharmacy (particularly those taking opioids, anti-coagulants, and/or antibiotics); and those with comorbidities like cardiovascular disease, hypertension, diabetes, and behavioral health. Nurses and organizations that identify and assess at-risk patient populations can increase the opportunity for good outcomes.
- Each nurse is only as good as their team. The decisions and behaviors of each team member impact the individual nurse’s ability to succeed and the patient’s ability to thrive. The data highlights the importance of effective teamwork and team communication.